As reported in The Age, 18.5.2018 https://www.theage.com.au/politics/act/assisted-dying-an-ill-considered-and-dehumanising-practice-archbishop-20180518-p4zg5p.html
Assisted dying is an “ill-considered and dehumanising” practice reflecting a society in which there is more loneliness, Canberra’s Catholic archbishop Christopher Prowse has told an inquiry.
He spoke at an ACT Legislative Assembly committee’s second day of hearings into assisted dying in which doctors rubbished claims that palliative care could always manage end of life pain.
Archbishop Prowse told the committee it was a “lonely policy that only an atomised society would think about”, and said people approaching death experienced a “rollercoaster” that saw them take back comments they wanted to die earlier.
He said it would be a “fundamental mistake” to put vulnerable people at “grave risk” by allowing assisted dying.
When asked what was a good death, Archbishop Prowse recounted a time he sat with a woman as she died, and she squeezed his hand.
“I could tell she was on a journey but how grateful she was when she was with us,” he said.
“She was ready to go, ready to go and approach death.”
He admitted people he had spent time with as they were dying had said they wanted to die right away. However they changed their mind later, he said.
“Then people say, ‘I’m feeling a lot better today’.”
Ian Wood responds to Archbishop Prowse, as follows ……
Archbishop C. Prowse, Canberra, ACT
I refer to the report of your evidence given to the ACT Assisted Dying hearing as reported in The Age, 18.5.2018.
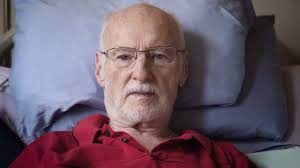
Keith, described here by his wife, was on a “journey” too, but was certainly not “grateful” to still be alive “with us”! (See attachment 1 below.)
You ignore the fact that over 1/3 of terminal patients in Oregon USA, who are given access to voluntary assisted dying medication, at their considered, repeated rational request, do not go on to take that fatal medication, but it does provide peace of mind in that they can choose to exit life if the suffering becomes unbearable. Having access is palliative in its own right.
Certainly when my sister-in-law Joyce died from ovarian cancer that had spread to her bones, she was not capable of squeezing any hands during her last two days! She said goodbye to her husband and family on a Sunday afternoon, but lingered on in a semi coma for another two days. In moments of lucidity she would ask why am I still here? Her husband is still suffering from the trauma of watching these last days. How much better and more compassionate it would have been for Joyce if she could have asked for, and been given medication to assist her to go to sleep and not wake up, after those final goodbyes.
The truly vulnerable are those who Continue reading